Hair loss is one of the most feared side effects. But not all chemotherapy causes baldness. Some medications target rapidly dividing cells aggressively. Others are milder and don’t affect hair much. Modern regimens consider patient comfort and appearance. Scalp cooling systems also help preserve follicles during treatment. The idea of inevitable baldness is outdated.
Radiation therapy is often thought to burn the skin severely
Older equipment had less precision. Skin burns were more common decades ago. Today’s machines focus beams tightly on the tumor. The surrounding healthy skin gets far less exposure. Side effects may include redness or dryness, but rarely burns. These effects fade shortly after treatment ends. The horror stories are mostly from past eras.
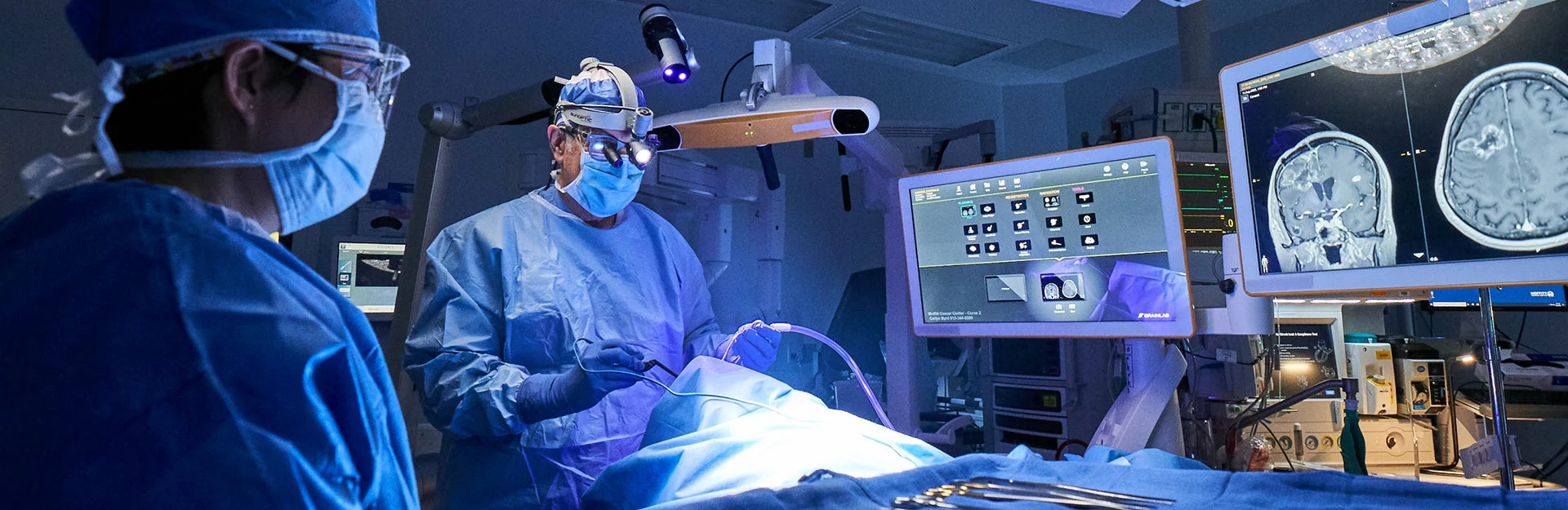
People assume surgery spreads cancer cells throughout the body
This myth causes many patients to delay life-saving operations. But there’s no scientific basis. Surgery doesn’t make cancer worse. In fact, removing tumors early increases survival chances. Surgeons follow strict protocols to prevent cell displacement. Delays caused by this fear often lead to advanced stages. The risk lies in waiting, not in operating.
Immunotherapy is not just about boosting the immune system blindly
Some think it’s like taking vitamins or herbal boosters. It’s far more targeted. Immunotherapy trains the body to recognize cancer cells as enemies. It uses engineered proteins or cell therapies. These approaches are complex and precise. General immune stimulation doesn’t work the same way. Misunderstanding this causes people to undervalue new treatments.
Cancer is not a death sentence in most modern cases
Survival rates have increased steadily over the years. Early detection plays a major role. So do targeted therapies and improved surgical techniques. Many cancers are manageable long-term. Some enter remission for decades. Yet fear lingers due to outdated perceptions. Public awareness hasn’t caught up with medical progress.
Natural treatments are often believed to replace clinical therapies
Many patients turn to herbs or diets instead of treatment. This approach can be dangerous. Natural remedies may interfere with actual medication. Some delay chemotherapy or surgery, hoping food alone can cure. Evidence doesn’t support these alternatives as standalone options. Supplements should only be used alongside approved therapies.
Biopsies don’t cause cancer to spread in the body
Some worry that testing tissue can activate cancer cells. This is not supported by data. Biopsies use fine needles or minimal incisions. Their purpose is accurate diagnosis. Without them, treatment plans lack focus. Avoiding biopsies based on myth delays critical care. Most specialists insist on samples for safe decision-making.
Not all tumors are treated with chemotherapy
People often assume chemo is always the first step. But treatments vary by cancer type. Some respond better to radiation or immunotherapy. Others require surgery alone. Chemotherapy is part of many plans, but not all. Doctors tailor combinations based on individual biology. The “chemo by default” mindset is misleading.
Targeted therapy doesn’t destroy everything like traditional drugs do
Old drugs attacked both healthy and cancerous cells. Targeted therapy acts more like a sniper. It blocks specific mutations or pathways cancer uses to grow. Side effects are usually milder than chemo. These treatments come after genetic analysis of the tumor. Not all patients are eligible, but many benefit.
Side effects don’t always indicate treatment failure
Some patients stop treatment if they feel worse. But reactions don’t mean the drug isn’t working. Inflammation, fatigue, or nausea may reflect the body’s response. Doctors manage these effects with supportive care. Stopping too early wastes potential benefit. Tracking progress with scans gives a better picture.
Young people can and do get cancer
There’s a belief that cancer only strikes the old. That’s not always true. Certain cancers, like lymphoma or sarcoma, often affect younger patients. Genetics and environmental exposure matter too. Dismissing symptoms because of age delays diagnosis. Awareness campaigns now focus on early signs in all age groups.
Once cancer is gone, follow-up is still critical
Some patients stop seeing their oncologist after remission. That’s risky. Cancer can return without warning. Follow-up scans and blood tests detect recurrence early. Long-term care includes managing late effects of treatment. Lifelong monitoring helps preserve health. Victory over cancer doesn’t end with the last session.
Clinical trials aren’t just for hopeless cases
Some believe trials are only for terminal patients. That’s false. Many trials test new drugs in early stages. Others compare standard treatments to newer ones. Participants often receive cutting-edge care. Trials are regulated and safe. They give access to medications not yet available widely.
Cancer doesn’t always require aggressive treatment
Not every diagnosis leads to intense intervention. Some tumors grow slowly or stay localized. In certain cases, “watchful waiting” is preferred. Doctors monitor growth before acting. This avoids overtreatment and side effects. Each case needs individual evaluation. More is not always better in oncology.
Hormone therapy isn’t exclusive to breast cancer
People associate hormone-blocking drugs with breast cancer alone. But prostate cancer also responds to these treatments. Hormone-sensitive tumors shrink when hormone levels drop. Blocking receptors or suppressing production slows the disease. This approach is essential in many long-term plans. It’s broader than most realize.
Chemotherapy doesn’t always weaken the immune system drastically
It depends on the drug and dosage. Some regimens reduce white blood cells sharply. Others have minimal effect. Doctors monitor counts regularly. Patients may receive growth factors to restore immunity. Infection risk exists but is manageable. The image of a completely defenseless patient is exaggerated.
Secondary cancers are rare but monitored
Radiation and chemo carry long-term risks. Secondary malignancies can develop years later. However, they’re rare. Benefits usually outweigh these risks. Doctors plan treatment with this in mind. Monitoring continues for decades. The goal is always maximum safety with effective results.
People still believe stress alone causes cancer
Stress affects health but doesn’t directly cause tumors. It can weaken the immune system. But cancer involves genetic mutations and environmental triggers. Blaming stress oversimplifies a complex disease. Managing anxiety is useful but not curative. Clear thinking is essential during treatment.
Cancer is not contagious in any form
This myth still circulates in some regions. No cancer type spreads from person to person. It’s not caused by viruses directly, except in rare cases like HPV. Sharing meals or living together is safe. Stigma causes patients to feel isolated unnecessarily. Education helps end this fear.
Eating sugar doesn’t feed cancer cells selectively
All cells need glucose, not just cancerous ones. Reducing sugar may help general health. But starving the body won’t kill tumors. Strict sugar avoidance lacks scientific support. Balanced nutrition supports treatment better. Malnutrition weakens healing. Diet choices should be guided by professionals.